Care for your patients and your practice
Discover a faster, more effective way to collect patient payments and maintain practice profitability — without sacrificing patient experience.
Finally: A smarter patient payment solution
Managing patient billing efficiently and effectively is one of the largest hurdles to practice profitability. We’ve made it easy to overcome those obstacles.
Solution built for a new era of patient pay
Navigating the complexities of medical billing is challenging for practices and patients alike – and the stakes for getting it right continue to increase. PatientFocus services were born from an enduring commitment to improve the medical billing journey for both practices and patients. The result of that commitment? Patient-pay solution options deliver faster payments to support practice cash flow, and a better overall patient experience.
Bring clarity to patient payment chaos
Streamline and synchronize your patient payment systems.
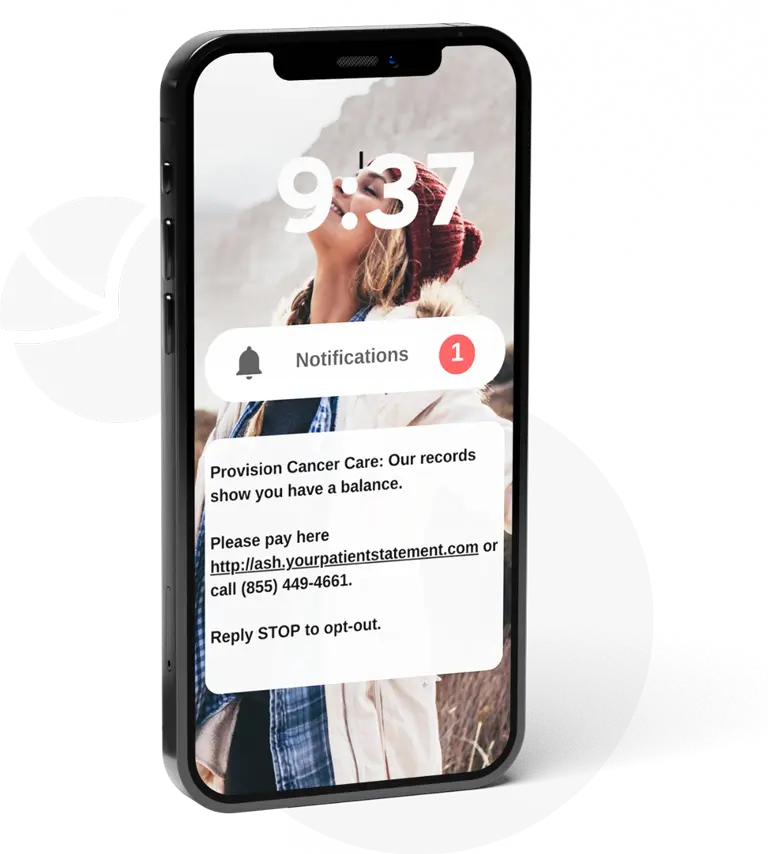
Juggling multiple systems for patient payments leads to inefficiencies and operational chaos. PatientFocus offers a single, seamless platform that unifies all aspects of patient billing and communications. Our omni-channel approach ensures that every patient interaction is optimized for ease and effectiveness, enhancing satisfaction and boosting your collections. With patient-pay analytics, gain insights needed to make informed decisions and keep your financial goals in focus.
Patient pay solutions that delivers on profitability and patient experience
Practice survival hinges on robust patient payment strategies — delays and non-payments can cripple cash flow and overall profitability. Our solutions are specifically designed to increase collection rates and decrease time-to-payment.
Clear benefits for every role in healthcare
Client success stories
Discover why practices choose to partner with PatientFocus for their patient bill solution.
“Working smarter not harder means partnering with best of breed vendors to bring their expertise to our process. PatientFocus’s medical billing services have allowed us to standardize our AR outreach across practices while modernizing the patient experience.”
Terrill Jordan, President and CEO
Regional Cancer Care Associates
“We needed an efficient, cost-effective means of collecting numerous small-balance bills. Using ‘their tools, our rules’, PatientFocus lets us increase revenue and minimize the day-to-day responsibilities associated with patient pay billing management. It has proven to be a great partnership.”
Jon Grimes, CEO
Optimal Radiology
“We partnered with PatientFocus because they understand the importance of the patient relationship. PatientFocus was certainly able to increase revenues and support our billing office, but the ability to treat our patients with the respect, fairness and empathy we require has been of utmost significance.”
Jinfer Cross, Leader, AR Management
e+CancerCare



